UPPER LIMB
OSCE
Station 6
Flexors of the Forearm and Hand
The flexor muscles of the forearm are in the anterior compartment and are separated from the posterior extensor compartment by the radius, ulnar and interosseous membrane. The flexor muscles are divided into two groups: the superficial and deep layers. The superficial group of muscles arise as a common flexor origin from the medial epicondyle of the humerus and cross the elbow joint whereas, the deep group of muscles arise from the radius, ulnar or interosseous membrane.
From radial to ulnar the muscles in the superficial layer are:
- Pronator teres.
- Flexor carpi radialis.
- Flexor digitorum superficialis (can be considered as an ‘intermediate’ layer).
- Palmaris longus.
- Flexor carpi ulnaris.
The deep layer of forearm flexor muscles comprise of:
- Flexor pollicis longus.
- Flexor digitorum profundus.
- Pronator quadratus.
What is the nerve supply to the flexor muscles of the forearm?
All muscles in the anterior (flexor) compartment are supplied by the median nerve with the exception of flexor carpi ulnaris and flexor digitorum profundus to the little and ring fingers.
Note: The deep group of muscles are supplied by the anterior interosseous nerve which is a branch of the median nerve.
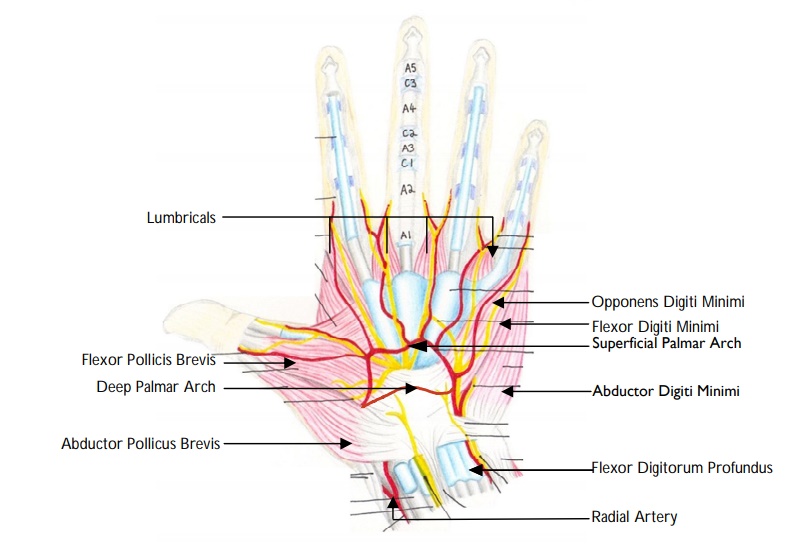
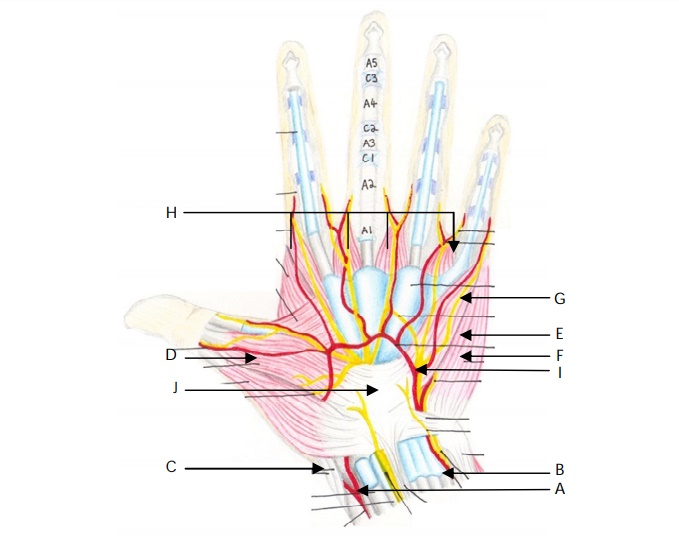
The lumbrical muscles arise from the radial aspect of the FDP tendons in the palm. They insert into the extensor expansions on the dorsum of the digits near the MCPJs.
Note: Therefore the lumbricals flex the digits at the MCPJs and extend the interphalangeal joints.
""The flexor pollicis longus is the only tendon that flexes the interphalangeal joint of the thumb. It can be tested by holding the proximal phalanx of the thumb and asking the patient to flex the distal interphalangeal joint."
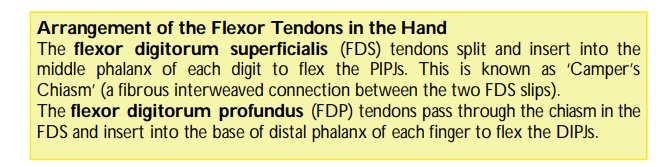
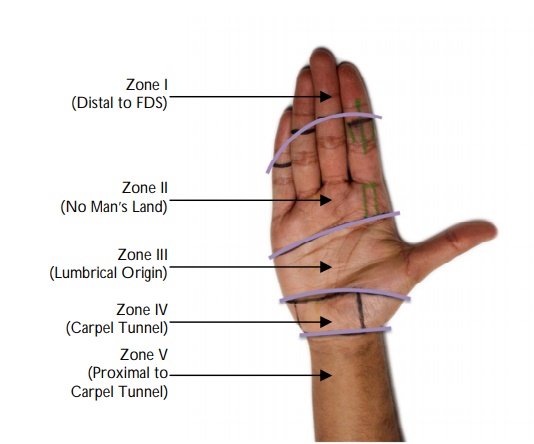
Zone I : Distal to the insertion of FDS.
Zone II : FDS insertion to proximal end of A1 pulley.
Zone III : Mid-palm (from the proximal aspect of the A1 pulley to the distal end of flexor retinaculum).
Zone IV : Under the flexor retinaculum (transverse carpal ligament).
Zone V : From the proximal end of flexor retinaculum (corresponds to distal wrist crease) to the forearm.
Note: Zone II injuries are often referred to as ‘No Man’s Land’ because repair in this zone is very difficult.
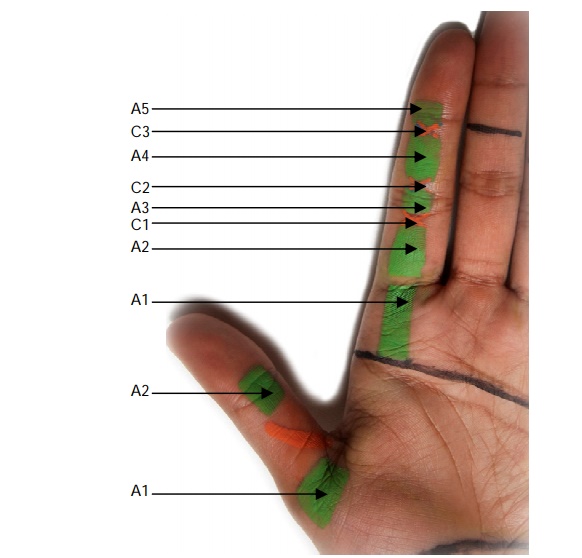
The flexor tendons run in a fibrous sheath which is constructed of segments of thickened fibrous solid tunnels (known as annular pulleys) and interlinking collapsible areas (known as cruciate pulleys). The annular pulleys are found over the shafts of the phalanges and the cruciate pulleys over the joints:
A1 : Over the MCPJ.
A2 : Over the proximal phalanx.
C1 : Between A2 and A3.
A3 : Over the PIPJ.
C2 : Between A3 and A4.
A4 : Over middle phalanx.
C3 : Between A4 and A5.
A5 : Over the DIPJ.
Note: The pulley’s often referred to as the ‘critical pulleys’ (as they prevent bowstringing) are the annular pulleys, particularly A2 and A4.
Palmaris longus (absent in approximately 10-15% of the population) can be harvested for a tendon graft and is often used for reconstruction.
Note: It ends in the fan-shaped palmar fascia.
"The palmar aponeurosis (palmar fascia) is made up of three layers:
- A superficial layer containing longitudinal fibres.
- An intermediate layers containing transverse fibres.
- A deep layer containing vertical fibres.
Conditions associated with Dupuytren’s disease include:
Garrod’s pads: knuckle pads.
Peyronie’s disease: penile fibrous plaques.
Ledderhosen’s disease: plantar fibromatosis.
"Trigger finger, also known as stenosing tenosynovitis, is due to a mismatch between a thickened or stenotic first annular (A1) pulley in the hand and the flexor tendon trying to glide through the pulley. This causes the flexor tendon to catch or lock proximal interphalangeal joint as the patient attempts to extend the finger, results in difficulty flexing or extending the finger known as the ‘triggering’ phenomenon.
"