UPPER LIMB
OSCE
Station 5
The Wrist
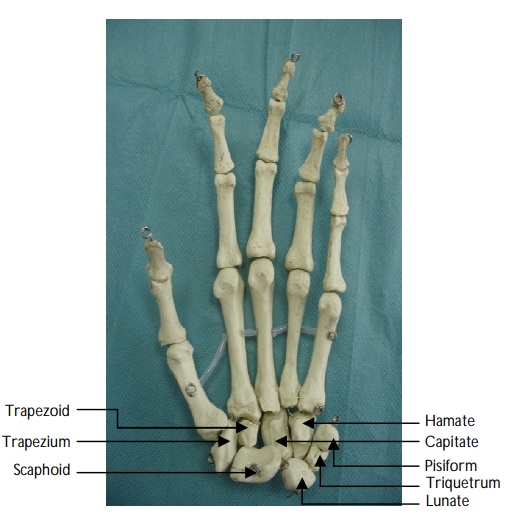
Identify the proximal and distal rows of carpal bones on the image:
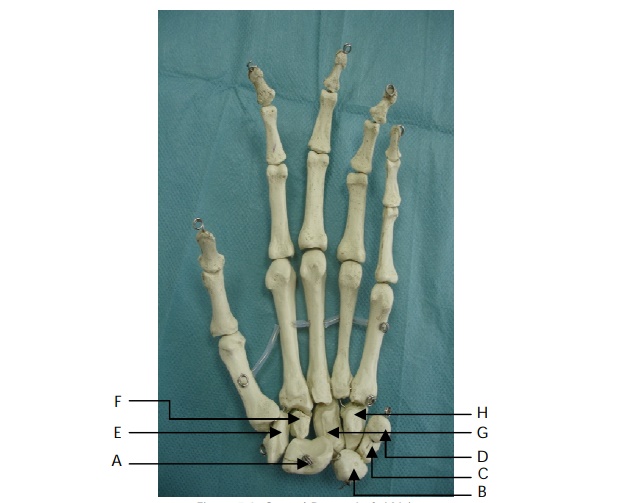
Proximal row:
A Scaphoid
B Lunate
C Triquetrum
D Pisiform
Distal row:
E Trapezium
F Trapezoid
G Capitate
H Hamate
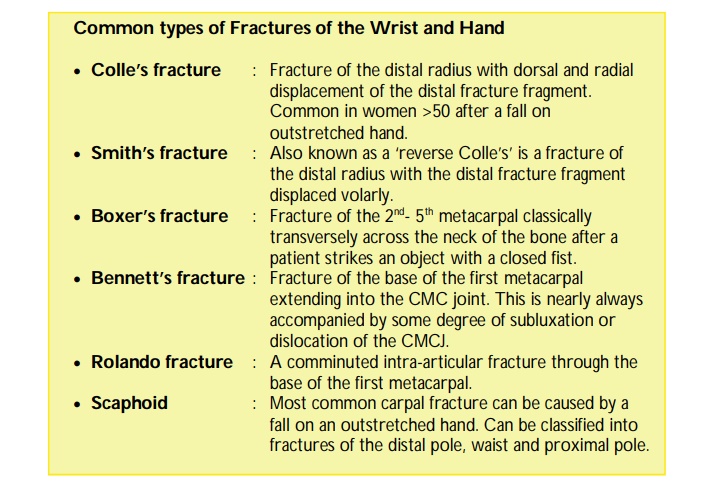
The blood supply enters the scaphoid via branches from the radial artery from distal to proximal. A fracture through the waist of the scaphoid disrupts this blood supply and can lead to avascular necrosis of the proximal aspect of the scaphoid.
Note: This may present many months after the original injury as pain and stiffness in the wrist.
Tenderness in the anatomical snuffbox and/ or base of the thumb is suggestive of a fracture of the scaphoid.
Early identification; fractures may not be visualized on initial plain radiographs (‘scaphoid views’). MRI can be useful to evaluate a fracture of the scaphoid if there is high index of suspicion and initial X-rays are negative.
"
- Clinically suspicious but normal X-ray:
- Immobilise in short arm thumb spica for 2/52. Review and repeat X-ray. If there is no tenderness in the anatomical snuffbox and repeat X-ray is normal, then no further treatment is required.
- Fracture confirmed on X-ray:
- Undisplaced and distal pole or waist fracture: Scaphoid cast for 6 weeks. For proximal pole fractures: Consider percutaneous or internal fixation.
- Displaced fractures: Early surgical fixation (percutaneous or open reduction and internal fixation).
"
| Guyon’s canal (or ulnar canal) is the space at the wrist between the pisiform and hamate, through which the ulnar artery and ulnar nerve enter the hand. |
"
Guyon's canal syndrome is caused by entrapment of the ulnar nerve in Guyon’s canal as it passes through the wrist leading to numbness in the little finger and ulnar half of the ring finger. It can progress to impaired intrinsic motor function.
Note: Guyon’s canal syndrome is commonly seen in cyclists due to prolonged pressure of Guyon’s canal against bicycle handlebars. It may also be caused by a wrist ganglion pressing on the motor branch of the ulnar nerve in the canal, in which case there is no sensory deficit.
"
"
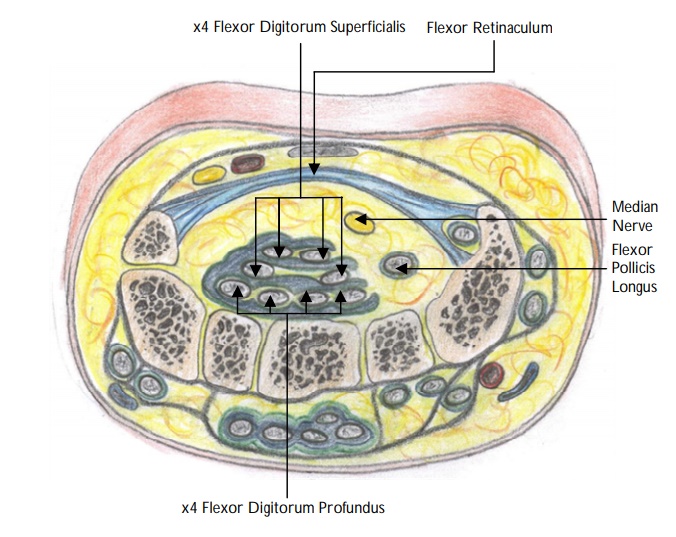
Roof : Flexor retinaculum (transverse carpal ligament).
Floor : Carpal bones.
"
"
- Hook of the hamate and pisiform on the ulnar side.
- Tubercle of the scaphoid and the ridge of the trapezium on the radial side.
"
| Ten structures pass through the carpal tunnel. |
"
- Median nerve.
- 4 x Flexor digitorum superficialis tendons.
- 4 x Flexor digitorum profundus tendons.
- Flexor pollicis longus tendon.
Note that the motor ‘recurrent’ branch of the median nerve arises under or distal to the flexor retinaculum to supply the thenar eminence and radial two lumbricals.
"
Palmaris longus tendon (when present).
Palmar cutaneous branch of the median nerve.
Superficial branch of the radial artery.
Note: The ulnar nerve and artery enter the hand through Guyon’s canal. Thus, for descriptive purposes, they run above the retinaculum
If pressure increases within the carpal tunnel, there is little room for expansion against either the bones of the wrist or the flexor retinaculum and the median nerve can ultimately be compressed within the tunnel. This results in impaired sensation to median nerve territory and wasting of the thenar muscles.
Note: It commonly affects women (F:M ratio = 8:1) aged 30-60.
The structures at risk during carpal tunnel decompression are the:
Palmar cutaneous branch of the median nerve.
Recurrent branch of the median nerve.
Median nerve.
Superficial palmar arch.
Flexor tendons.
Ulnar nerve and artery (if the incision is placed too ulnar).
"
- The deep palmar arch is formed by the continuation of the terminal (deep) branch of the radial artery that enters the palm after piercing the first dorsal interossei. It anastomoses with the superficial branch of the ulnar artery to form the deep palmar arch, which lies in the plane of a line drawn along the radial border of the fully extended thumb.
- The superficial palmar is formed predominantly by the deep branch of the ulnar artery which anastomoses with the superficial palmar branch of the radial artery which lies just distal to a line drawn from the ulnar border of the thumb to the hook of hamate (Kaplan’s cardinal line).
"
| The anterior and posterior interosseous arteries (from the common interosseous artery which arises from the ulnar artery supply the distal radioulnar joint. It is innervated by the anterior and posterior interosseous nerves (from the median and radial nerves respectively). |
"
- The distal radioulnar joint is a pivot type of synovial joint. The radius moves around the relatively fixed distal end of the ulna. The rounded head of the ulna articulates with the ulna notch on the distal end of the radius. A fibrocartilaginous articular disc ‘triangular ligament’ binds the ends of the ulna and radius together. The articular disc separates the cavity of the distal radioulnar joint from the cavity of the wrist joint.
- The fibrous capsule encloses the distal radioulnar joint but is deficient superiorly: this accommodates the twisting of the capsule that occurs when the distal end of the radius travels around the relatively fixed distal end of the ulnar during pronation. Anterior and posterior ligaments strengthen the fibrous capsule of the distal radioulnar joint. During pronation and supination of the forearm and hand, the distal end of the radius moves anteriorly and medially, crossing the ulnar anteriorly.
"
The superficial palmar arch lies distal to this line, and can be injured by incisions that cross the line. Surgical incisions for carpal tunnel decompression and for access to the wrist should therefore be placed proximal to this line.
