THORAX
OSCE
Station 9
The Anatomy of Central Line Insertion
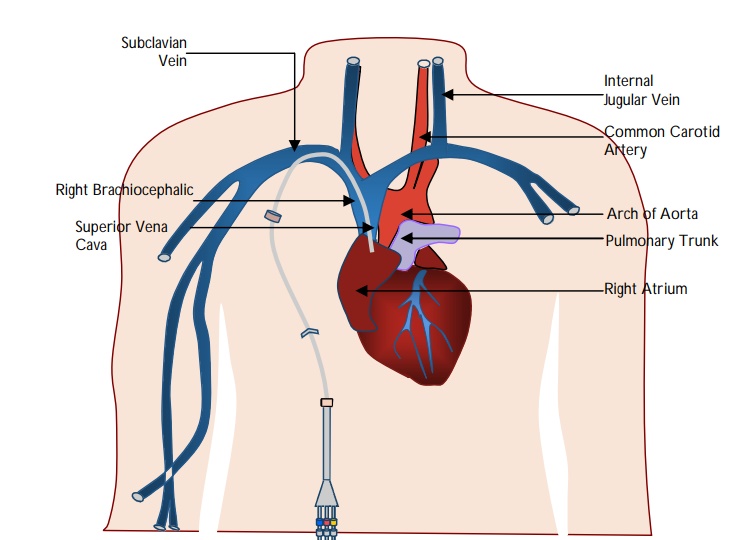
The root of the neck is the junction between the neck and thorax and contains all structures passing between the neck and thorax:
- Arteries: Common carotid (right and left), subclavian arteries (right and left)
- Veins: Right and left IJV and subclavian veins forming the (right and left brachiocephalic veins).
- Trachea
- Oesophagus
- Vagus nerves
- Phrenic nerves
- Thymus gland
The stellate ganglion:
- Lies anterior to the transverse process of C7.
- Superior to the neck of the 1st rib.
- Just below the subclavian artery.
- The vertebral artery lies anterior to the ganglion as it has just originated from the subclavian artery.
- Excision of the ganglion (sympathectomy) is performed to minimise symptoms associated with Raynaud’s phenomenon, hyperhidrosis (specifically in palmar hyperhidrosis) and facial blushing. This is usually performed endoscopically.
- Local anaesthetic block (stellate ganglion block) can be performed by injecting near the stellate ganglion to minimise sympathetically medicated pain such as complex regional pain syndrome.
- The inferior petrosal sinus and the sigmoid sinus join at the base of the brain to form the internal jugular vein (IJV) and exits the skull through the jugular foramen.
- The right and left IJV unites with the corresponding subclavian vein to form the brachiocephalic vein.
- The right and the left brachiocephalic veins unite to form the superior vena cava.
- The IJV lies in the anterior triangle of the neck.
- The carotid sheath lies just in front of the anterior border of sternocleidomastoid muscle (SCM)
- The IJV may lies within the carotid sheath (along with the internal carotid artery and vagus nerve).
- The carotid artery lies anteromedially within the sheath.
Note: The needle should be inserted pointing towards the ipsilateral nipple. The carotid artery should be identified and gently moved medially to avoid inadvertent cannulation.
"- The IJV lies lateral and inferior to the junction of the sternal and clavicular heads of sternocleidomastoid.
- The pleura lies inferomedial and the subclavian artery lies lateral to the IJV.
- The IJV drains into the brachiocephalic vein. On the right this is shorter and drains more vertically into the superior vena cava (therefore making it easier to cannulate).
The vagus nerve lies between the internal jugular vein and the carotid artery in the neck.
The subclavian vein can be identified as it follows the course of the subclavian artery in the neck, curving laterally over the apex of the lung to reach the 1st rib.
The subclavian vein lies anterior to insertion of scalenus anterior on the first rib (artery lies posterior).
The needle is advanced initially at the junction of the outer and middle 1/3rd of the clavicle at 45°, then directed towards the suprasternal notch.
Indications for insertion of a central venous catheter include:
- Frequent or persistent requirement for intravenous access.
- Long term intravenous fluids and drug administration.
- For patients requiring frequent blood monitoring.
- Chemotherapy/administration of drugs prone to be toxic to peripheral veins (e.g., vasopressors).
- Haemodialysis/ haemofiltration.
- Monitoring of the central venous pressure (CVP).
Complications of insertion of internal jugular vein cannulation include:
Immediate:
Injury to local structures resulting in:
Bleeding (risk of significant haemorrhage from the carotid artery).
Pseudoaneurysm.
Pneumothorax.
Haemothorax.
Chylothorax (specifically on the left side due to presence of the thoracic duct).
Nerve injuries (in particular brachial plexus and vagus nerve).
Cardiac arrhythmias.
Air embolism.
Retention of guide wire.
Late:
Sepsis.
Thromboembolism.
AV fistula formation.